Myopia Management Solutions
MYOPIA DEFINITION
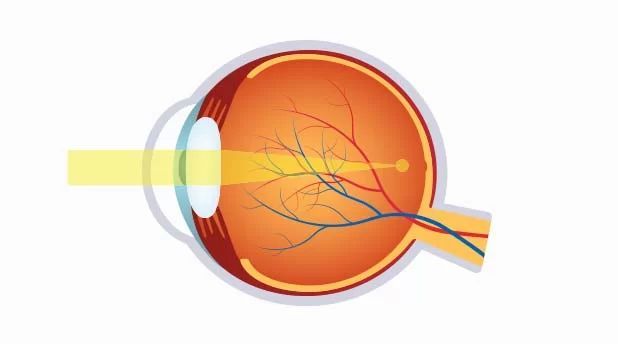
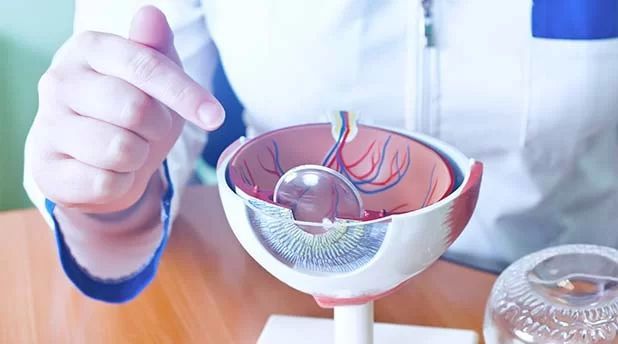
People with myopia have difficulty seeing objects further away. Nearsightedness, or myopia, as it is medically termed, is a vision condition in which near objects are seen clearly, but distant objects do not come into proper focus.
Nearsightedness occurs if your eyeball is too long or the cornea has too much curvature, so the light entering your eye is not focused correctly. Nearsightedness is a very common vision condition that affects nearly 30 percent of the U.S. population. Some evidence supports the theory that nearsightedness is hereditary.

MYOPIA CAUSES
There is also growing evidence that nearsightedness may be caused by the stress of too much close vision work. It normally first occurs in school-age children. Because the eye continues to grow during childhood, nearsightedness generally develops before age 20.
A sign of nearsightedness is difficulty seeing distant objects like a movie or TV screen or chalkboard. A comprehensive optometric examination will include testing for nearsightedness. Your optometrist can prescribe eyeglasses or contact lenses to optically correct nearsightedness by altering the way the light images enter your eyes.

MYOPIA TREATMENT
You may only need to wear them for certain activities, like watching TV or a movie or driving a car, or they may need to be worn for all activities. Refractive surgery or laser procedures are also possible treatments for nearsightedness as is orthokeratology.
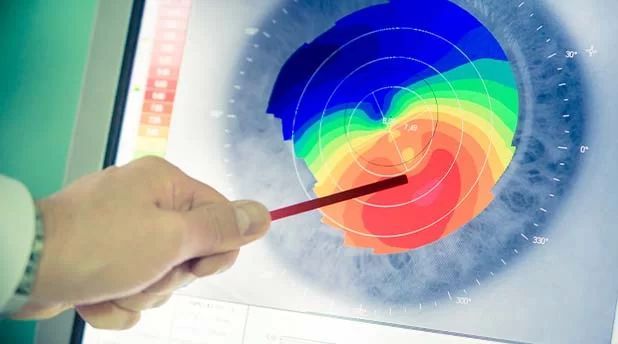
Orthokeratology (ortho-k) is a non-invasive procedure that involves the wearing of a series of specially-designed rigid contact lenses to progressively reshape the curvature of the cornea over time.

In Americans aged 12 to 54 years, the prevalence of myopia has almost doubled to over 40% in the past 30 years (Vitale et al, 2009).

High myopia is strongly linked to a higher risk of cataracts, retinal detachment, and myopic maculopathy (Flitcroft, 2012). Increasing rates of vision impairment and blindness due to the latter are already evident in Asian countries (Iwase et al, 2006; Wu et al, 2011).
Even 1.00D of myopia doubles the risk of myopic maculopathy (MM) and posterior subcapsular cataract (PSCC) and triples the risk of retinal detachment (RD) compared to emmetropes (not requiring correction).

At 3.00D of myopia, the risk of PSCC triples, and the risk of RD and MM is nine times that of an emmetrope. Once children reach 5.00D of myopia, they hold a five times greater risk of PSCC, a 21 times greater risk of RD, and a 40 times greater risk of MM; higher levels bring more eye-watering risks. These ratio risks demonstrate that there is no physiological level of myopia that could be considered “safe” in comparison to emmetropia (Flitcroft, 2012)
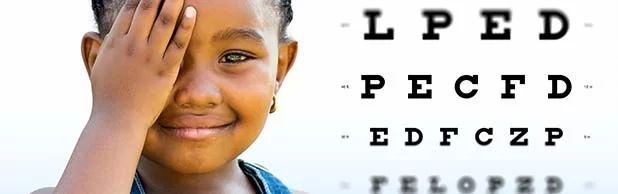
However, myopia control is not just applicable to myopes; exhibiting less than 0.50D of manifest hyperopia at age 6 to 7 years is the most significant risk factor for future myopia, independent of family history and visual environment (Zadnik et al, 2015).

The fastest rate of refractive change in myopic children occurs in the year prior to onset (Mutti et al, 2007), so children who are less hyperopic than age normal should be closely monitored, especially if concurrent risk factors of family history or binocular vision status are evident.

Children who have one myopic parent have a three-fold risk of myopia development compared to their peers who do not have this family history; two myopic parents double this risk again (Jones et al, 2007).

Initiating a myopia management strategy for pediatric patients should ideally commence before they become myopic, in view of the risk factors described above.

CLAMP
Walline JJ, Jones LA, Mutti DO, and Zanik K: A Randomized Trial of the Effect of Rigid Contact Lenses on Myopia Progression. Arch Ophthalmol 122: 1760-1766, 2004
(Contact Lens And Myopia Progression) Jeff Walline studied 59 RGP eyes versus 57 soft lens eyes. There was no difference in axial length growth. RGPs flattened the cornea .5D, while soft lenses steepened it .5D. GPs slowed progression but only a small amount.

COMET
(Correction of Myopia Evaluation Trial) Progressive Addition Lenses slowed myopic progression by .13D over five years, an effect considered negligible. Gwiazda J, Hyman L, Hussein M, Everett D, Norton TT, Kurtz D, Leske MC, Manny R, Marsh-Tootle W, Scheiman M, and the COMET Group: A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children.
CRAYON
Not yet been published. Walline, Jeffrey J., Slowing Myopia Progression Spectrum, June 2007.
(Corneal Reshaping and Yearly Observation of Nearsightedness) An update to the LORIC study. Jeff Walline. CR slows axial growth over the study length of two years.

COOKI
Children’s Overnight Orthokeratology Investigation
Essentially proved that CR works overnight for children in the 8-11-year-old group. Invest Ophthalmol Vis Sci 2003;44:
SMART
(Stabilization of Myopia through Accelerated Reshaping Technologies) In a five-year study where after each year of wear the patient is allowed to normalize without wearing their molding lenses after which they start wearing their lenses again. Preliminary results show stability after one year. The EyeVis Eye and Vision Research Institute.

CANDY
The study graph below summarizes the data. David Bartels and Peter Wilcox (Controlling Astigmatism and Nearsightedness in Developing Youth) Showed myopic progression of -.37D per year in normally corrected myopes and -.03D per year in CR patients. Patients were allowed to normalize at various times during their CR wear.
